Botulism
| Botulism | |
|---|---|
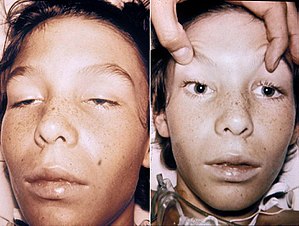 | |
| A 14-year-old with botulism. Note the weakness of his eye muscles and the drooping eyelids in the adjacent image, and the large and non moving pupils in the right image. This youth was fully conscious. | |
| Pronunciation |
|
| Specialty | Infectious disease, gastroenterology |
| Symptoms | Weakness, trouble seeing, feeling tired, trouble speaking[1] |
| Complications | Respiratory failure[2] |
| Usual onset | 12 to 72 hours[2] |
| Duration | Variable[2] |
| Causes | Clostridium botulinum[1] |
| Diagnostic method | Finding the bacteria or their toxin[1] |
| Differential diagnosis | Myasthenia gravis, Guillain–Barré syndrome, Amyotrophic lateral sclerosis, Lambert Eaton syndrome[3] |
| Prevention | Proper food preparation, no honey for children less than one[1] |
| Treatment | Antitoxin, antibiotics, mechanical ventilation[1] |
| Prognosis | ~7.5% risk of death[1] |
Botulism is a rare and potentially fatal illness caused by a toxin produced by the bacterium Clostridium botulinum.[1] The disease begins with weakness, blurred vision, feeling tired, and trouble speaking.[1] This may then be followed by weakness of the arms, chest muscles, and legs.[1] Vomiting, swelling of the abdomen, and diarrhea may also occur.[1] The disease does not usually affect consciousness or cause a fever.[1]
Botulism can be spread in several different ways.[1] The bacterial spores which cause it are common in both soil and water.[1] They produce the botulinum toxin when exposed to low oxygen levels and certain temperatures.[1] Foodborne botulism happens when food containing the toxin is eaten.[1] Infant botulism happens when the bacteria develops in the intestines and releases the toxin.[1] This typically only occurs in children less than six months old, as protective mechanisms develop after that time.[1] Wound botulism is found most often among those who inject street drugs.[1] In this situation, spores enter a wound, and in the absence of oxygen, release the toxin.[1] It is not passed directly between people.[1] The diagnosis is confirmed by finding the toxin or bacteria in the person in question.[1]
Prevention is primarily by proper food preparation.[1] The toxin, though not the organism, is destroyed by heating it to more than 85 °C (185 °F) for longer than 5 minutes.[1]Honey can contain the organism, and for this reason, honey should not be fed to children under 12 months.[1] Treatment is with an antitoxin.[1] In those who lose their ability to breathe on their own, mechanical ventilation may be necessary for months.[1]Antibiotics may be used for wound botulism.[1] Death occurs in 5 to 10% of people.[1] Botulism also affects many other animals.[1] The word is from Latin, botulus, meaning sausage.[4] Early descriptions of botulism date from at least as far back as 1793 in Germany.[5]
Contents
1 Signs and symptoms
1.1 Infant botulism
1.2 Complications
2 Cause
2.1 Colonization of the gut
2.2 Food
2.3 Wound
2.4 Inhalation
2.5 Injection
3 Mechanism
4 Diagnosis
5 Prevention
5.1 Vaccine
6 Treatment
6.1 Antitoxin
7 Prognosis
8 Epidemiology
8.1 United States
8.2 United Kingdom
8.3 China
8.4 Canada
8.5 Ukraine
9 Other species
10 See also
11 References
12 External links
Signs and symptoms
The muscle weakness of botulism characteristically starts in the muscles supplied by the cranial nerves—a group of twelve nerves that control eye movements, the facial muscles and the muscles controlling chewing and swallowing. Double vision, drooping of both eyelids, loss of facial expression and swallowing problems may therefore occur. In addition to affecting the voluntary muscles, it can also cause disruptions in the autonomic nervous system. This is experienced as a dry mouth and throat (due to decreased production of saliva), postural hypotension (decreased blood pressure on standing, with resultant lightheadedness and risk of blackouts), and eventually constipation (due to decreased forward movement of intestinal contents).[6] Some of the toxins (B and E) also precipitate nausea, vomiting,[6] and difficulty with talking. The weakness then spreads to the arms (starting in the shoulders and proceeding to the forearms) and legs (again from the thighs down to the feet).[6]
Severe botulism leads to reduced movement of the muscles of respiration, and hence problems with gas exchange. This may be experienced as dyspnea (difficulty breathing), but when severe can lead to respiratory failure, due to the buildup of unexhaled carbon dioxide and its resultant depressant effect on the brain. This may lead to respiratory compromise and death if untreated.[6]
Clinicians frequently think of the symptoms of botulism in terms of a classic triad: bulbar palsy and descending paralysis, lack of fever, and clear senses and mental status ("clear sensorium").[7]
Infant botulism

Infant with botulism. He is unable to move or open his eyes. His cry was weak. He is not asleep or sedated.
Infant botulism (also referred to as floppy baby syndrome) was first recognized in 1976, and is the most common form of botulism in the United States. Infants are susceptible to infant botulism in the first year of life, with more than 90% of cases occurring in infants younger than six months.[8] Infant botulism results from the ingestion of the C. botulinum spores, and subsequent colonization of the small intestine. The infant gut may be colonized when the composition of the intestinal microflora (normal flora) is insufficient to competitively inhibit the growth of C. botulinum and levels of bile acids (which normally inhibit clostridial growth) are lower than later in life.[9]
The growth of the spores releases botulinum toxin, which is then absorbed into the bloodstream and taken throughout the body, causing paralysis by blocking the release of acetylcholine at the neuromuscular junction. Typical symptoms of infant botulism include constipation, lethargy, weakness, difficulty feeding and an altered cry, often progressing to a complete descending flaccid paralysis. Although constipation is usually the first symptom of infant botulism, it is commonly overlooked.[10]
Honey is a known dietary reservoir of C. botulinum spores and has been linked to infant botulism. For this reason honey is not recommended for infants less than one year of age.[9] Most cases of infant botulism, however, are thought to be caused by acquiring the spores from the natural environment. Clostridium botulinum is a ubiquitous soil-dwelling bacterium. Many infant botulism patients have been demonstrated to live near a construction site or an area of soil disturbance.[11]
Infant botulism has been reported in 49 of 50 US states (all save for Rhode Island),[8] and cases have been recognized in 26 countries on five continents.[12]
Complications
Infant botulism has no long-term side effects, but can be complicated by hospital-acquired infections.
Botulism can result in death due to respiratory failure. However, in the past 50 years, the proportion of patients with botulism who die has fallen from about 50% to 7% due to improved supportive care. A patient with severe botulism may require mechanical ventilation (breathing support through a ventilator) as well as intensive medical and nursing care, sometimes for several months. The person may require rehabilitation therapy after leaving the hospital.[13]
Cause

A photomicrograph of Clostridium botulinum bacteria.
Clostridium botulinum is an anaerobic, Gram positive, spore-forming rod. Botulinum toxin is one of the most powerful known toxins: about one microgram is lethal to humans when inhaled.[14] It acts by blocking nerve function (neuromuscular blockade) through inhibition of the excitatory neurotransmitter acetylcholine's release from the presynaptic membrane of neuromuscular junctions in the somatic nervous system. This causes paralysis. Advanced botulism can cause respiratory failure by paralysing the muscles of the chest; this can progress to respiratory arrest.[15] Furthermore, acetylcholine release from the presynaptic membranes of muscarinic nerve synapses is blocked. This can lead to a variety of autonomic signs and symptoms described above.
In all cases, illness is caused by the botulinum toxin produced by the bacterium C. botulinum in anaerobic conditions and not by the bacterium itself. The pattern of damage occurs because the toxin affects nerves that fire (depolarize) at a higher frequency first.[16]
Mechanisms of entry into the human body for botulinum toxin are described below.
Colonization of the gut
The most common form in Western countries is infant botulism. This occurs in infants who are colonized with the bacterium in the small intestine during the early stages of their lives. The bacterium then produces the toxin, which is absorbed into the bloodstream. The consumption of honey during the first year of life has been identified as a risk factor for infant botulism; it is a factor in a fifth of all cases.[6] The adult form of infant botulism is termed adult intestinal toxemia, and is exceedingly rare.[6]
Food
Toxin that is produced by the bacterium within containers of food that have been improperly preserved is the most common cause of food-borne botulism. Fish that has been pickled without the salinity or acidity of brine that contains acetic acid and high sodium levels, as well as smoked fish stored at too high a temperature, presents a risk, as does improperly canned food.
Food-borne botulism results from contaminated food in which C. botulinum spores have been allowed to germinate in low-oxygen conditions. This typically occurs in home-canned food substances and fermented uncooked dishes.[17] Given that multiple people often consume food from the same source, it is common for more than a single person to be affected simultaneously. Symptoms usually appear 12–36 hours after eating, but can also appear within 6 hours to 10 days.[18]
Wound
Wound botulism results from the contamination of a wound with the bacteria, which then secrete the toxin into the bloodstream. This has become more common in intravenous drug users since the 1990s, especially people using black tar heroin and those injecting heroin into the skin rather than the veins.[6] Wound botulism accounts for 29% of cases.
Inhalation
Isolated cases of botulism have been described after inhalation by laboratory workers.
Injection
Botulism has occurred after cosmetic use of inappropriate strengths of Botox.[6]
Mechanism
The toxin is the protein botulinum toxin produced under anaerobic conditions (where there is no oxygen) by the bacterium Clostridium botulinum.
Clostridium botulinum is a large anaerobic Gram-positive bacillus that forms subterminal endospores.[19]
There are eight serological varieties of the bacterium denoted by the letters A to H. The toxin from all of these acts in the same way and produces similar symptoms: the motor nerve endings are prevented from releasing acetylcholine, causing flaccid paralysis and symptoms of blurred vision, ptosis, nausea, vomiting, diarrhea or constipation, cramps, and respiratory difficulty.
Botulinum toxin is broken into 8 neurotoxins (labeled as types A, B, C [C1, C2], D, E, F, and G), which are antigenically and serologically distinct but structurally similar. Human botulism is caused mainly by types A, B, E, and (rarely) F. Types C and D cause toxicity only in other animals.[20]
In October 2013, scientists released news of the discovery of type H, the first new botulism neurotoxin found in forty years. However, further studies showed type H to be a chimeric toxin composed of parts of types F and A (FA).[21]
Some types produce a characteristic putrefactive smell and digest meat (types A and some of B and F); these are said to be proteolytic; type E and some types of B, C, D and F are nonproteolytic and can go undetected because there is no strong odor associated with them.[19]
When the bacteria are under stress, they develop spores, which are inert. Their natural habitats are in the soil, in the silt that comprises the bottom sediment of streams, lakes and coastal waters and ocean, while some types are natural inhabitants of the intestinal tracts of mammals (e.g., horses, cattle, humans), and are present in their excreta. The spores can survive in their inert form for many years.[22]
Toxin is produced by the bacteria when environmental conditions are favourable for the spores to replicate and grow, but the gene that encodes for the toxin protein is actually carried by a virus or phage that infects the bacteria. Unfortunately, little is known about the natural factors that control phage infection and replication within the bacteria.[23]
The spores require warm temperatures, a protein source, an anaerobic environment, and moisture in order to become active and produce toxin. In the wild, decomposing vegetation and invertebrates combined with warm temperatures can provide ideal conditions for the botulism bacteria to activate and produce toxin that may affect feeding birds and other animals. Spores are not killed by boiling, but botulism is uncommon because special, rarely obtained conditions are necessary for botulinum toxin production from C. botulinum spores, including an anaerobic, low-salt, low-acid, low-sugar environment at ambient temperatures.[24]
Botulinum inhibits the release within the nervous system of acetylcholine, a neurotransmitter, responsible for communication between motor neurons and muscle cells. All forms of botulism lead to paralysis that typically starts with the muscles of the face and then spreads towards the limbs.[6] In severe forms, botulism leads to paralysis of the breathing muscles and causes respiratory failure. In light of this life-threatening complication, all suspected cases of botulism are treated as medical emergencies, and public health officials are usually involved to identify the source and take steps to prevent further cases from occurring.[6]
Botulinum toxin A, C, and E cleave the SNAP-25, ultimately leading to paralysis.
Diagnosis
For botulism in babies, diagnosis should be made on signs and symptoms. Confirmation of the diagnosis is made by testing of a stool or enema specimen with the mouse bioassay.
Physicians may consider diagnosing botulism if the patient's history and physical examination suggest botulism. However, these clues are often not enough to allow a diagnosis. Other diseases such as Guillain–Barré syndrome, stroke, and myasthenia gravis can appear similar to botulism, and special tests may be needed to exclude these other conditions. These tests may include a brain scan, cerebrospinal fluid examination, nerve conduction test (electromyography, or EMG), and an edrophonium chloride (Tensilon) test for myasthenia gravis. A definite diagnosis can be made if botulinum toxin is identified in the food, stomach or intestinal contents, vomit or feces. The toxin is occasionally found in the blood in peracute cases. Botulinum toxin can be detected by a variety of techniques, including enzyme-linked immunosorbent assays (ELISAs), electrochemiluminescent (ECL) tests and mouse inoculation or feeding trials. The toxins can be typed with neutralization tests in mice. In toxicoinfectious botulism, the organism can be cultured from tissues. On egg yolk medium, toxin-producing colonies usually display surface iridescence that extends beyond the colony.[25]
Prevention
Although the vegetative form of the bacteria is destroyed by boiling,[26][27] the spore itself is not killed by the temperatures reached with normal sea-level-pressure boiling, leaving it free to grow and again produce the toxin when conditions are right.[28][29]
A recommended prevention measure for infant botulism is to avoid giving honey to infants less than 12 months of age, as botulinum spores are often present. In older children and adults the normal intestinal bacteria suppress development of C. botulinum.[30]
While commercially canned goods are required to undergo a "botulinum cook" in a pressure cooker at 121 °C (250 °F) for 3 minutes, and thus rarely cause botulism, there have been notable exceptions. Two were the 1978 Alaskan salmon outbreak and the 2007 Castleberry's Food Company outbreak. Foodborne botulism is the rarest form though, accounting for only around 15% of cases (US)[31] and has more frequently been from home-canned foods with low acid content, such as carrot juice, asparagus, green beans, beets, and corn. However, outbreaks of botulism have resulted from more unusual sources. In July 2002, fourteen Alaskans ate muktuk (whale meat) from a beached whale, and eight of them developed symptoms of botulism, two of them requiring mechanical ventilation.[32]
Other, much rarer sources of infection (about every decade in the US[31]) include garlic or herbs[33] stored covered in oil without acidification,[34]chili peppers,[31] improperly handled baked potatoes wrapped in aluminum foil,[31] tomatoes,[31] and home-canned or fermented fish.
When canning or preserving food at home, attention should be paid to hygiene, pressure, temperature, refrigeration and storage. When making home preserves, only acidic fruit such as apples, pears, stone fruits and berries should be bottled. Tropical fruit and tomatoes are low in acidity and must have some acidity added before they are bottled.[35]
Low-acid foods have pH values higher than 4.6. They include red meats, seafood, poultry, milk,
and all fresh vegetables except for most tomatoes. Most mixtures of low-acid and acid foods also
have pH values above 4.6 unless their recipes include enough lemon juice, citric acid, or vinegar
to make them acid foods. Acid foods have a pH of 4.6 or lower. They include fruits, pickles,
sauerkraut, jams, jellies, marmalades, and fruit butters.[36]
Although tomatoes usually are considered an acid food, some are now known to have pH values
slightly above 4.6. Figs also have pH values slightly above 4.6. Therefore, if they are to be canned
as acid foods, these products must be acidified to a pH of 4.6 or lower with lemon juice or citric
acid. Properly acidified tomatoes and figs are acid foods and can be safely processed in a
boiling-water canner.[36]
Oils infused with fresh garlic or herbs should be acidified and refrigerated. Potatoes which have been baked while wrapped in aluminum foil should be kept hot until served or refrigerated. Because the botulism toxin is destroyed by high temperatures, home-canned foods are best boiled for 10 minutes before eating.[37] Metal cans containing food in which bacteria, possibly botulinum, are growing may bulge outwards due to gas production from bacterial growth; such cans should be discarded.[38]
Any container of food which has been heat-treated and then assumed to be airtight which shows signs of not being so, e.g., metal cans with pinprick holes from rust or mechanical damage, should be discarded. Contamination of a canned food solely with C. botulinum may not cause any visual defects (e.g. bulging). Only sufficient thermal processing during production should be used as a food safety control.
Vaccine
There is a vaccine but its usefulness is unclear as it is associated with significant adverse effects.[1] As of 2013 there are efforts ongoing to develop a better vaccine.[39]
Treatment
Botulism is generally treated with botulism antitoxin and supportive care.[1]
Supportive care for botulism includes monitoring of respiratory function. Respiratory failure due to paralysis may require mechanical ventilation for 2 to 8 weeks, plus intensive medical and nursing care. After this time, paralysis generally improves as new neuromuscular connections are formed.[40]
In some abdominal cases, physicians may try to remove contaminated food still in the digestive tract by inducing vomiting or using enemas. Wounds should be treated, usually surgically, to remove the source of the toxin-producing bacteria.[41]
Antitoxin
Botulinum antitoxin consists of antibodies that neutralize botulinum toxin in the circulatory system by passive immunization.[42] This prevents additional toxin from binding to the neuromuscular junction, but does not reverse any already inflicted paralysis.[42]
In adults, a trivalent antitoxin containing antibodies raised against botulinum toxin types A, B, and E is used most commonly, however a heptavalent botulism antitoxin has also been developed and was approved by the U.S. FDA in 2013.[15][43] In infants, horse-derived antitoxin is sometimes avoided for fear of infants developing serum sickness or lasting hypersensitivity to horse-derived proteins.[44] To avoid this, a human-derived antitoxin has been developed and approved by the U.S. FDA in 2003 for the treatment of infant botulism.[45] This human-derived antitoxin has been shown to be both safe and effective for the treatment of infant botulism.[45][46] However, the danger of equine-derived antitoxin to infants has not been clearly established, and one study showed the equine-derived antitoxin to be both safe and effective for the treatment of infant botulism.[44]
Trivalent (A,B,E) botulinum antitoxin is derived from equine sources utilizing whole antibodies (Fab and Fc portions). In the United States, this antitoxin is available from the local health department via the CDC. The second antitoxin, heptavalent (A,B,C,D,E,F,G) botulinum antitoxin, is derived from "despeciated" equine IgG antibodies which have had the Fc portion cleaved off leaving the F(ab')2 portions. This less immunogenic antitoxin is effective against all known strains of botulism where not contraindicated.[citation needed]
Prognosis
The paralysis caused by botulism can persist for 2 to 8 weeks, during which supportive care and ventilation may be necessary to keep the person alive.[40] Botulism is fatal in 5% to 10% of people who are affected.[1] However, if left untreated, botulism is fatal in 40% to 50% of cases.[46]
Infant botulism typically has no long-term side effects but can be complicated by treatment associated adverse events. The case fatality rate is less than 1% for hospitalized babies.[citation needed]
Epidemiology
Globally, botulism is fairly rare,[1] with approximately 1,000 cases yearly.[47]
United States
In the United States an average of 145 cases are reported each year. Of these, roughly 65% are infant botulism, 20% are wound botulism, and 15% are foodborne.[48] Infant botulism is predominantly sporadic and not associated with epidemics, but great geographic variability exists. From 1974 to 1996, for example, 47% of all infant botulism cases reported in the U.S. occurred in California.[48]
Between 1990 and 2000, the Centers for Disease Control and Prevention reported 263 individual foodborne cases from 160 botulism events in the United States with a case-fatality rate of 4%. Thirty-nine percent (103 cases and 58 events) occurred in Alaska, all of which were attributable to traditional Alaska aboriginal foods. In the lower 49 states, home-canned food was implicated in 70 (91%) events with canned asparagus being the most numerous cause. Two restaurant-associated outbreaks affected 25 persons. The median number of cases per year was 23 (range 17–43), the median number of events per year was 14 (range 9–24). The highest incidence rates occurred in Alaska, Idaho, Washington, and Oregon. All other states had an incidence rate of 1 case per ten million people or less.[49]
The number of cases of food borne and infant botulism has changed little in recent years, but wound botulism has increased because of the use of black tar heroin, especially in California.[50]
All data regarding botulism antitoxin releases and laboratory confirmation of cases in the US are recorded annually by the Centers for Disease Control and Prevention and published on their website.[48]
1971 Bon Vivant botulism case On July 2, 1971, the U.S. Food and Drug Administration (FDA) released a public warning after learning that a New York man had died and his wife had become seriously ill due to botulism after eating a can of Bon Vivant vichyssoise soup.- Between March 31 and April 6, 1977, 59 individuals developed type B botulism. All ill persons had eaten at the same Mexican restaurant in Pontiac, Michigan and all had consumed a hot sauce made with improperly home-canned jalapeño peppers, either by adding it to their food, or by eating a nacho that had had hot sauce used in its preparation. The full clinical spectrum (mild symptomatology with neurologic findings through life-threatening ventilatory paralysis) of type B botulism was documented.[51]
- In April 1994, the largest outbreak of botulism in the United States since 1978 occurred in El Paso, Texas. Thirty persons were affected; 4 required mechanical ventilation. All ate food from a Greek restaurant. The attack rate among persons who ate a potato-based dip was 86% (19/22) compared with 6% (11/176) among persons who did not eat the dip (relative risk [RR] Å 13.8; 95% confidence interval [CI], 7.6–25.1). The attack rate among persons who ate an eggplant-based dip was 67% (6/9) compared with 13% (24/189) among persons who did not (RR Å 5.2; 95% CI, 2.9–9.5). Botulism toxin type A was detected from patients and in both dips. Toxin formation resulted from holding aluminum foil-wrapped baked potatoes at room temperature, apparently for several days, before they were used in the dips. Food handlers should be informed of the potential hazards caused by holding foil-wrapped potatoes at ambient temperatures after cooking.[52]
- In 2002, fourteen Alaskans ate muktuk (whale blubber) from a beached whale, resulting in eight of them developing botulism, with two of the affected requiring mechanical ventilation.[53]
- Beginning in late June 2007, 8 people contracted botulism poisoning by eating canned food products produced by Castleberry's Food Company in its Augusta, Georgia plant. It was later identified that the Castleberry's plant had serious production problems on a specific line of retorts that had under-processed the cans of food. These issues included broken cooking alarms, leaking water valves and inaccurate temperature devices, all the result of poor management of the company. All of the victims were hospitalized and placed on mechanical ventilation. The Castleberry's Food Company outbreak was the first instance of botulism in commercial canned foods in the United States in over 30 years.[citation needed]
- One person died, 21 cases were confirmed, and 10 more were suspected in Lancaster, Ohio when a botulism outbreak occurred after a church potluck in April 2015. The suspected source was a salad made from home-canned potatoes.[54]
- A botulism outbreak occurred in Northern California in May 2017 after 10 people consumed nacho cheese dip served at a gas station in Sacramento County. One man died as a result of the outbreak.[55]
United Kingdom
The largest recorded outbreak of foodborne botulism in the United Kingdom occurred in June 1989. A total of 27 patients were affected; one patient died. Twenty-five of the patients had eaten one brand of hazelnut yogurt in the week before the onset of symptoms. Control measures included the cessation of all yogurt production by the implicated producer, the withdrawal of the firm's yogurts from sale, the recall of cans of the hazelnut conserve, and advice to the general public to avoid the consumption of all hazelnut yogurts.[56]
China
From 1958–1983 there were 986 outbreaks of botulism in China involving 4,377 people with 548 deaths.[57]
Canada
From 1985-2015 there was an outbreak of 91 confirmed cases of foodborne botulism in Canada, 85% of which were in Inuit communities, especially Nunavik and First Nations of the coast of British Columbia from eating traditionally prepared marine mammal and fish products.[58]
Ukraine
In 2017, there were 70 cases of botulism with 8 deaths in Ukraine. The previous year there were 115 cases with 12 deaths.[59]
Other species
Botulism can occur in many vertebrates and invertebrates. Botulism has been reported in rats, mice, chicken, frogs, toads, goldfish, aplysia, squid, crayfish, drosophila, leeches, etc.[60]
Death from botulism is common in waterfowl; an estimated 10,000 to 100,000 birds die of botulism annually. The disease is commonly called "limberneck". In some large outbreaks, a million or more birds may die. Ducks appear to be affected most often. An enzootic form of duck botulism in Western USA and Canada is known as "western duck sickness".[61] Botulism also affects commercially raised poultry. In chickens, the mortality rate varies from a few birds to 40% of the flock.
Botulism seems to be relatively uncommon in domestic mammals; however, in some parts of the world, epidemics with up to 65% mortality are seen in cattle. The prognosis is poor in large animals that are recumbent.
In cattle, the symptoms may include drooling, restlessness, uncoordination, urine retention, dysphagia, and sternal recumbency. Laterally recumbent animals are usually very close to death. In sheep, the symptoms may include drooling, a serous nasal discharge, stiffness, and incoordination. Abdominal respiration may be observed and the tail may switch on the side. As the disease progresses, the limbs may become paralyzed and death may occur.
Phosphorus-deficient cattle, especially in southern Africa, are inclined to ingest bones and carrion containing clostridial toxins and consequently suffer lame sickness or lamsiekte.
A recent study has demonstrated an effective vaccine against cattle botulism associated with Clostridium botulinum serotypes C and D.[62]
The clinical signs in horses are similar to cattle. The muscle paralysis is progressive; it usually begins at the hindquarters and gradually moves to the front limbs, neck, and head. Death generally occurs 24 to 72 hours after initial symptoms and results from respiratory paralysis. Some foals are found dead without other clinical signs.
Clostridium botulinum type C toxin has been incriminated as the cause of grass sickness, a condition in horses which occurs in rainy and hot summers in Northern Europe. The main symptom is pharynx paralysis.[63]
Domestic dogs may develop systemic toxemia after consuming C. botulinum type C exotoxin or spores within bird carcasses or other infected meat[64] but are generally resistant to the more severe effects of Clostridium botulinum type C.
Symptoms include flaccid muscle paralysis; dogs with breathing difficulties will require more intensive care monitoring. Muscle paralysis can lead to death due to cardiac and respiratory arrest.[65]
Pigs are relatively resistant to botulism. Reported symptoms include anorexia, refusal to drink, vomiting, pupillary dilation, and muscle paralysis.[66]
In poultry and wild birds, flaccid paralysis is usually seen in the legs, wings, neck and eyelids. Broiler chickens with the toxicoinfectious form may also have diarrhea with excess urates.
See also
- List of foodborne illness outbreaks
References
^ abcdefghijklmnopqrstuvwxyzaaabacadaeafag "Botulism Fact sheet N°270". World Health Organization. October 2017. Archived from the original on 11 October 2017. Retrieved 17 November 2017..mw-parser-output cite.citation{font-style:inherit}.mw-parser-output q{quotes:"""""""'""'"}.mw-parser-output code.cs1-code{color:inherit;background:inherit;border:inherit;padding:inherit}.mw-parser-output .cs1-lock-free a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-subscription a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration{color:#555}.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration span{border-bottom:1px dotted;cursor:help}.mw-parser-output .cs1-hidden-error{display:none;font-size:100%}.mw-parser-output .cs1-visible-error{font-size:100%}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-format{font-size:95%}.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-left{padding-left:0.2em}.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-right{padding-right:0.2em}
^ abc "Consumers - Foodborne Illnesses: What You Need to Know". FDA. Retrieved 11 May 2018.
^ Caterino, Jeffrey M.; Kahan, Scott (2003). In a Page: Emergency medicine. Lippincott Williams & Wilkins. p. 122. ISBN 9781405103572. Archived from the original on 2017-09-10.
^ Lewis, Charlton T.; Short, Charles. "A Latin Dictionary". Archived from the original on 2014-08-14. Retrieved 2014-06-09.
^ Truong, Daniel; Dressler, Dirk; Hallett, Mark; Zachary, Christopher (2014). Manual of Botulinum Toxin Therapy (2 ed.). Cambridge University Press. p. 1. ISBN 9781107654334. Archived from the original on 2017-09-10.
^ abcdefghij Sobel, J. (2005). "Botulism". Clinical Infectious Diseases. 41 (8): 1167–73. doi:10.1086/444507. PMID 16163636.
^ "Botulism". OutbreakID.com. Archived from the original on 2 April 2012.
^ ab Arnon SS (2004). "Infant Botulism". In Feigin RD; Cherry JD; Demmler GJ; Kaplan SL. Textbook of Pediatric Infectious Diseases (PDF) (5th ed.). Philadelphia: WB Saunders. pp. 1758–66. Archived (PDF) from the original on 2011-07-26.
^ ab Caya, James G.; Agni, Rashmi; Miller, Joan E. (2004). "Clostridium botulinum and the Clinical Laboratorian: A Detailed Review of Botulism, Including Biological Warfare Ramifications of Botulinum Toxin". Archives of Pathology & Laboratory Medicine. 128 (6): 653–62. doi:10.1043/1543-2165(2004)128<653:CBATCL>2.0.CO;2. PMID 15163234. Retrieved 21 June 2016.
^ "Infant Botulism". kidshealth.org. Archived from the original on 2016-10-07. Retrieved 2016-09-28.
^ Domingo, Rose M; Haller, Jerome S; Gruenthal, Michael (1 Nov 2008). "Infant Botulism: Two recent cases and a literature review". Journal of Child Neurology. 23 (11): 1340. doi:10.1177/0883073808318200.
^ Koepke, R.; Sobel, J.; Arnon, S. S. (2008). "Global Occurrence of Infant Botulism, 1976–2006". Pediatrics. 122 (1): e73–e82. doi:10.1542/peds.2007-1827. PMID 18595978.
^ "Clostridium perfringens". U.S. Centers for Disease Control and Prevention. Archived from the original on 16 June 2016. Retrieved 14 June 2016.
^ Donald Emmeluth (2010). Botulism. Infobase Publishing. p. 38. ISBN 978-1-60413-235-9. Archived from the original on 2017-01-01.
^ ab Arnon, Stephen S.; Schechter, Robert; Inglesby, Thomas V.; Henderson, Donald A.; Bartlett, John G.; Ascher, Michael S.; Eitzen, Edward; Fine, Anne D.; Hauer, Jerome; Layton, Marcelle; Lillibridge, Scott; Osterholm, Michael T.; O'Toole, Tara; Parker, Gerald; Perl, Trish M.; Russell, Philip K.; Swerdlow, David L.; Tonat, Kevin (2001). "Botulinum toxin as a biological weapon: medical and public health management". JAMA. 285 (8): 1059–70. doi:10.1001/jama.285.8.1059. PMID 11209178.
^ Oxford Textbook of Medicine, 4th Ed., Section 7.55
^ "Botulism, General Information". Centers for Disease Control and Prevention. Archived from the original on 2016-08-03. Retrieved 2016-08-05.
^ "Facts About Botulism". Emergency Preparedness and Response. Centers for Disease Control and Prevention. October 14, 2001. Archived from the original on July 5, 2011. Retrieved July 2, 2011.
^ ab "ETOX 80E -Botulism". University of California, Santa Cruz. Archived from the original on 2013-05-09. Retrieved 2014-02-12.
^ Botulinum Toxin at eMedicine
^ A Novel Botulinum Neurotoxin, Previously Reported as Serotype H, Has a Hybrid-Like Structure With Regions of Similarity to the Structures of Serotypes A and F and Is Neutralized With Serotype A Antitoxin. Maslanka SE, Lúquez C, Dykes JK, Tepp WH, Pier CL, Pellett S, Raphael BH, Kalb SR, Barr JR, Rao A, Johnson EA. J Infect Dis. 2016 Feb 1; 213(3): 379–85
^ Ward, BQ; Carroll, BJ; Garrett, ES; Reese, GB (1967). "Survey of the U.S. Gulf Coast for the presence of Clostridium botulinum". Applied Microbiology. 15 (3): 629–36. PMC 546991. PMID 5340653.
^ Franson JC, Friend M. "38: Avian Botulism". Field Manual of Wildlife Disease (PDF). U.S. Geological Survey. ISBN 978-0-607-88096-0. Archived (PDF) from the original on 9 August 2016. Retrieved 14 June 2016.
^ International Commission on Microbiological Specifications for Foods (1996). "Clostridium botulinum". Microorganisms in Foods 5: Characteristics of Microbial Pathogens. Springer. pp. 66–111. ISBN 978-0-412-47350-0. quoted in Centers for Disease Control Prevention (CDC) (2012). "Botulism from drinking prison-made illicit alcohol – Utah 2011". MMWR. 61 (39): 782–84. PMID 23034585. Archived from the original on 2017-06-06.
^ Weber, JT (1994). "Botulism". In Hpeprich, PD. Infectious Diseases (5th ed.). J. B. Lippincott Company. pp. 1185–94.
^ "Botulism". WHO. Archived from the original on 2014-02-16. Retrieved 2014-02-12.
^ "Foodborne Botulism FAQ". Food Safety Authority of Ireland. November 15, 2011. Archived from the original on May 21, 2014. Retrieved 2014-05-20.
^ Teotonio, Isabel (February 21, 2008). "Couple suing over tainted juice". Toronto Star. Archived from the original on March 4, 2016.
^ "Guidance for Industry: Refrigerated Carrot Juice and Other Refrigerated Low-Acid Juices". FDA. June 2007. Archived from the original on 2015-09-24.
^ Arnon, Stephen S.; Midura, Thaddeus F.; Damus, Karla; Thompson, Barbara; Wood, Ronald M.; Chin, James (1979). "Honey and other environmental risk factors for infant botulism". The Journal of Pediatrics. 94 (2): 331–36. doi:10.1016/S0022-3476(79)80863-X. PMID 368301.
^ abcde "Arctic Investigations Program – DPEI". Centers for Disease Control and Prevention (CDC). 2011-04-01. Archived from the original on 2010-10-16. Retrieved 2014-02-12.
^ Centers for Disease Control and Prevention (CDC) (January 2003). "Outbreak of botulism type E associated with eating a beached whale – Western Alaska, July 2002". MMWR Morb. Mortal. Wkly. Rep. 52 (2): 24–26. PMID 12608715. Archived from the original on 2017-06-25.
^ "Oil Infusions and the Risk of Botulism". Safefood News. Colorado State University Cooperative Extension. 1998. Archived from the original on 4 April 2013.
^ Centers for Disease Control (CDC) (October 1985). "Update: international outbreak of restaurant-associated botulism – Vancouver, British Columbia, Canada". MMWR Morb. Mortal. Wkly. Rep. 34 (41): 643. PMID 3930945. Archived from the original on 2017-06-25.
^ "Botulism fact sheet". Department of Public Health, Western Australia. Archived from the original on 2013-12-30. Retrieved 2014-02-12.
^ ab "Complete Guide to Home Canning; Guide 1: Principles of Home Canning" (PDF). United States Department of Agriculture. Archived (PDF) from the original on 2018-01-27. Retrieved 2018-08-15.
^ U.S. Food and Drug Administration. "Bad Bug Book: Foodborne Pathogenic Microorganisms and Natural Toxins Handbook Clostridium botulinum". Archived from the original on 29 November 2012. Retrieved 12 January 2013.
^ Schneider, Keith R.; Silverberg, Rachael; Chang, Alexandra; Goodrich Schneider, Renée M. (9 January 2015). "Preventing Foodborne Illness: Clostridium botulinum". edis.ifas.ufl.edu. University of Florida IFAS Extension. Archived from the original on 8 February 2017. Retrieved 7 February 2017.
^ Webb, Robert P; Smith, Leonard A (2013). "What next for botulism vaccine development?". Expert Review of Vaccines. 12 (5): 481–92. doi:10.1586/erv.13.37. PMID 23659297.
^ ab "Botulism: Treatment Overview for Clinicians". U.S. Centers for Disease Control and Prevention (CDC). 2006. Archived from the original on 4 March 2016. Retrieved 13 January 2016.
^ Brook, Itzhak (2006). "Botulism: the challenge of diagnosis and treatment". Reviews in Neurological Diseases. 3 (4): 182–89. PMID 17224901.
^ ab O’Horo, John C; Harper, Eugene P; El Rafei, Abdelghani; Ali, Rashid; DeSimone, Daniel C; Sakusic, Amra; Abu Saleh, Omar M; Marcelin, Jasmine R; Tan, Eugene M; Rao, Agam K; Sobel, Jeremy; Tosh, Pritish K (2018). "Efficacy of Antitoxin Therapy in Treating Patients With Foodborne Botulism: A Systematic Review and Meta-analysis of Cases, 1923–2016". Clinical Infectious Diseases. 66 (suppl_1): S43–S56. doi:10.1093/cid/cix815. ISSN 1058-4838.
^ "FDA approves first Botulism Antitoxin for use in neutralizing all seven known botulinum nerve toxin serotypes". FDA News Release. U.S. FDA. 22 March 2013. Archived from the original on 1 January 2016. Retrieved 14 January 2016.
^ ab Vanella de Cuetos EE; Fernandez RA; Bianco MI; Sartori OJ; Piovano ML; Luquez C; de Jong LIT (November 2011). "Equine Botulinum Antitoxin for the Treatment of Infant Botulism". Clin Vaccine Immunol. 18 (11): 1845–49. doi:10.1128/CVI.05261-11. PMC 3209035. PMID 21918119.
^ ab Arnon SS; Schechter R; Maslanka SE; Jewell NP; Hatheway CL (2006). "Human Botulism Immune Globulin for the Treatment of Infant Botulism". New England Journal of Medicine. 354 (5): 462–71. doi:10.1056/NEJMoa051926. PMID 16452558.
^ ab Chalk, Colin H; Benstead, Tim J; Keezer, Mark; Chalk, Colin H (2014). "Medical treatment for botulism". The Cochrane Database of Systematic Reviews. 2 (2): CD008123. doi:10.1002/14651858.CD008123.pub3. PMID 24558013.
^ Care, Government of Ontario, Ministry of Health and Long-Term. "Botulism - Diseases and Conditions - Publications - Public Information - MOHLTC". www.health.gov.on.ca. Retrieved 2017-10-29.
^ abc "National Case Surveillance: National Botulism Surveillance | CDC National Surveillance". Centers for Disease Control and Prevention. 2013-06-25. Archived from the original on 2014-01-30. Retrieved 2014-02-12.
^ Sobel J, Tucker N, Sulka A, McLaughlin J, Maslanka S (September 2004). "Foodborne Botulism in the United States, 1990–2000". Emerging Infectious Diseases. Centers for Disease Control. 10 (9): 1606–11. doi:10.3201/eid1009.030745. PMC 3320287. PMID 15498163. Archived from the original on 24 June 2016. Retrieved 14 June 2016.
^ Passaro, Douglas J.; Werner, Benson; McGee, Jim; Mac Kenzie, William R.; Vugia, Duc J. (1998). "Wound Botulism Associated With Black Tar Heroin Among Injecting Drug Users". JAMA. 279 (11): 859–63. doi:10.1001/jama.279.11.859. PMID 9516001.
^ Terranova, William; Breman, Joel G.; Locey, Robert P.; Speck, Sarah (1978). "Botulism type B: epidemiologic aspects of an extensive outbreak". American Journal of Epidemiology. 108 (2): 150–56. doi:10.1093/oxfordjournals.aje.a112599. PMID 707476.
^ Angulo, F. J.; Getz, J.; Taylor, J. P.; Hendricks, K. A.; Hatheway, C. L.; Barth, S. S.; Solomon, H. M.; Larson, A. E.; Johnson, E. A.; Nickey, L. N.; Ries, A. A. (1998). "A Large Outbreak of Botulism: The Hazardous Baked Potato". Journal of Infectious Diseases. 178 (1): 172–77. doi:10.1086/515615. PMID 9652437.
^
Middaugh, J; Funk, B; Jilly, B; Maslanka, S; McLaughlin J (2003-01-17). "Outbreak of Botulism Type E Associated with Eating a Beached Whale --- Western Alaska, July 2002". Morbidity and Mortality Weekly Report. 52 (2): 24–26. PMID 12608715.
^ "1 dead in botulism outbreak linked to Ohio church potluck". CNNWIRE. CNN. 28 April 2015. Archived from the original on 22 July 2015. Retrieved 19 July 2015.
^ "Man dies in Sacramento county botulism outbreak from nacho cheese". KCRA. 22 May 2017. Archived from the original on 23 May 2017. Retrieved 22 May 2017.
^ O'Mahony, M; Mitchell, E; Gilbert, RJ; Hutchinson, DN; Begg, NT; Rodhouse, JC; Morris, JE (1990). "An outbreak of foodborne botulism associated with contaminated hazelnut yoghurt". Epidemiology and Infection. 104 (3): 389–95. doi:10.1017/s0950268800047403. PMC 2271776. PMID 2347382.
^ Ying, S.; Shuyan, C. (1986-11-01). "Botulism in China". Clinical Infectious Diseases. 8 (6): 984–990. doi:10.1093/clinids/8.6.984. ISSN 0162-0886.
^ Leclair, Daniel; Fung, Joe; Isaac-Renton, Judith L.; Proulx, Jean-Francois; May-Hadford, Jennifer; Ellis, Andrea; Ashton, Edie; Bekal, Sadjia; Farber, Jeffrey M. (June 2013). "Foodborne Botulism in Canada, 1985–2005". Emerging Infectious Diseases. 19 (6): 961–968. doi:10.3201/eid1906.120873. ISSN 1080-6040. PMC 3713816. PMID 23735780.
^ "Eight Ukrainians died of botulism in 2017". LB.ua. Retrieved 2017-10-29.
^ Humeau Y, Doussau F, Grant NJ, Poulain B (May 2000). "How botulinum and tetanus neurotoxins block neurotransmitter release". Biochimie. 82 (5): 427–46. doi:10.1016/S0300-9084(00)00216-9. PMID 10865130.
^ W.B. Gross (1984), Botulism, in "Diseases of poultry", ed. by M.S. Hofstad, Iowa State University Press, Ames, Iowa, USA;
ISBN 0-8138-0430-2, 8th ed., p. 257
^ OCunha CE, Moreira GM, Salvarani FM, et al. (Jan 2014). "Vaccination of cattle with a recombinant bivalent toxoid against botulism serotypes C and D." Vaccine. 32 (2): 214–16. doi:10.1016/j.vaccine.2013.11.025. PMID 24252701.
^ D.C. Blood, J.A. Henderson, O.M. Radostits (1979). Veterinary Medicine (5th ed.). London: Baillière Tindall. pp. 1060 (Grass sickness). ISBN 0-7020-07-18-8.CS1 maint: Uses authors parameter (link)
^ "Dogs / Botulism". Vet Book. 2012-08-12. Archived from the original on 2014-02-21. Retrieved 2013-08-23.
^ "Overview of botulism in poultry". Merck Manuals. 2012-03-31. Archived from the original on 2014-02-04. Retrieved 2013-08-23.
^ S.E. Aiello; A. Mays, eds. (1988). "Botulism". Merck Veterinary Manual (8th ed.). Whitehouse Station, NJ: Merck and Co. pp. 442–44.
External links
| Classification | D
|
|---|---|
| External resources |
|
Wikipedia's health care articles can be viewed offline with the Medical Wikipedia app.
- BOTULISM in the United States, 1889–1996. Handbook for Epidemiologists, Clinicians and Laboratory Technicians. Centers for Disease Control and Prevention. National Center for Infectious Diseases, Division of Bacterial and Mycotic Diseases 1998.
- NHS choices
- CDC Botulism: Control Measures Overview for Clinicians
- University of California, Santa Cruz Environmental toxicology – Botulism
- CDC Botulism FAQ
- FDA Clostridium botulinum Bad Bug Book
- USGS Avian Botulism